RESEARCH ARTICLE | https://doi.org/10.5005/jp-journals-10005-1983 |
Prevalence and Pattern of Non-syndromic Hypodontia among Adolescents in Southern Part of India
1India
2,4Department of Pedodontics and Preventive Dentistry, Kalinga Institute of Dental Sciences, Bhubaneswar, Odisha, India
3,6Department of Pedodontics and Preventive Dentistry, MNR Dental College and Hospital, Sangareddy, Telangana, India
5Sangareddy, Telangana, India
Corresponding Author: Brahmananda Dutta, Department of Pedodontics and Preventive Dentistry, Kalinga Institute of Dental Sciences, Bhubaneswar, Odisha, India, Phone: +919437284141, e-mail: bndutta69@gmail.com
How to cite this article Manasa Devi TL, Dutta B, Dwijendra KS, et al. Prevalence and Pattern of Non-syndromic Hypodontia among Adolescents in Southern Part of India. Int J Clin Pediatr Dent 2021;14(4):492–496.
Source of support: Nil
Conflict of interest: None
ABSTRACT
Background: Non-syndromic hypodontia is the most common developmental dental anomaly, but there is a paucity of literature on its prevalence and severity in the Indian population.
Aim and objectives: To estimate the prevalence of non-syndromic hypodontia among adolescent schoolchildren in the southern part of India.
Settings and design: This cross-sectional study was conducted in 20 schools from two states of southern India, named—Andhra Pradesh and Telangana. A total of 5,458 children in the age-group 13 to 15 years were selected.
Materials and methods: Clinical examination was carried out to check the absence of a permanent tooth and was confirmed by radiographic findings. The inclusion criterion was children with all the permanent teeth erupted (except third molars) and exclusion criteria were teeth missing due to reasons other than congenital agenesis. A Chi-square test was applied to check the significance.
Results: The total prevalence of hypodontia in the study sample was 1.4%. Girls displayed a higher prevalence value (1.9%) than boys (1.1%). Maxillary lateral incisor was the most commonly congenitally missing tooth, followed by mandibular incisors and mandibular second premolar. Overall, hypodontia with a predominance of unilateral pattern and a predilection for the left side was observed.
Conclusion: The most common missing permanent tooth (except third molars) was the maxillary lateral incisor. Hypodontia was more prevalent in females and had a predominance of unilateral patterns with a predilection toward the left side.
Keywords: Congenitally missing tooth, Non-syndromic hypodontia, Tooth agenesis.
INTRODUCTION
Hypodontia is reported as the most common developmental dental anomaly in human beings.1–5 Few terminologies have been used to describe this condition such as “hypodontia” which is a clinical condition with a reduced number of tooth/teeth erupted into the oral cavity while the term “agenesis” refers to the failure of a tooth germ to develop in the oral cavity. The term “congenitally missing tooth” is a misnomer as tooth development is completed after birth and therefore, the absence of a tooth can only be ascertained postnatally.6–8 Although there is no consensus on the classification of hypodontia in the literature, the following terminologies have been used depending upon their clinical severity—Hypodontia denotes one to six teeth missing excluding third molars, condition presenting with more than six teeth missing excluding third molars is referred to as Oligodontia and the complete absence of teeth is termed Anodontia.9,10
Population studies have revealed that hypodontia may be manifested as an isolated finding or as part of a syndrome.11,12 Isolated forms may be sporadic or familial. Familial tooth agenesis is typically transmitted as an autosomal dominant trait with incomplete penetrance and variable expressivity.11,13 The defective genes associated with tooth agenesis as identified on gene mapping are MSX1, PAX9, AXIN2, LTBP3, and EDA.14 The role of environmental factors has been proven in studies conducted on monozygotic twins with congenitally missing teeth that showed disparities in the severity and clinical presentation of the condition.15,16 Maternal health has been considered a significant intrauterine factor and abnormal tooth agenesis has been reported in cases of Rubella, Rhesus-incompatibility, and Thalidomide embryopathy. Only those teeth that form early in development when compared with teeth whose formation is initiated after birth are likely to be affected by maternal health.7,17
Ectodermal dysplasia, incontinentia pigmenti, Witkop syndrome, Van Der Woude syndrome, Rieger syndrome, Down’s syndrome, and holoprosencephaly.9,10 Other dental anomalies that commonly coexist with syndromic hypodontia are microdontia, ectopic eruptions, transpositions, taurodontism, and reduction in alveolar growth thus, resulting in significant functional, esthetic, and psychological complications.11 An early and precise identification and intervention into the management of dental agenesis can prevent these complications.
The global data on the prevalence of hypodontia reveal a wide variation18 and may not apply to the Indian population with a diverse culture and ethnicity. Also, the published reports on Indian studies are scanty. Hence, considering the significance and paucity of data on hypodontia of the permanent dentition in the Indian population, with a diversity of culture and food habits, the present study was taken up.
AIM AND OBJECTIVE
To estimate the prevalence of non-syndromic hypodontia among adolescent schoolchildren in two southern states of India.
MATERIALS AND METHODS
The present cross-sectional study was completed over a period of 6 months. Ethical clearance was obtained from the Institutional Ethics Committee. The approval letter from the state education department for conducting the study was presented to the school authorities and permissions were obtained.
Study Population
Five districts (three from Andhra Pradesh and two from Telangana) were randomly selected based on the proportion of child population between the two states. Twenty schools, four from each district (2-government and 2-private) were considered following a simple random sampling technique. Initially, 5,773 students, studying in Standard: VIII–X and aged between 13 years and 15 years were screened and 5,458 children comprising 2,173 girls and 3,285 boys were included in this study.
Sample Size Determination
The sample size was derived using the formula Z2p(1 − p)/c2 and state child population census of the same age-group.
Inclusion and Exclusion Criteria
Inclusion criteria were physically and intellectually normal children without any developmental disorders with a complete set of permanent teeth (except third molars) erupted in the oral cavity. Children having clinically missing permanent teeth with/without over-retained primary predecessors were also included in this study. However, those who were in mixed dentition stages had a history of tooth loss as a result of extraction/trauma, and those undergoing fixed orthodontic treatment with extraction were excluded from the study.
Examination Procedure
A single clinician carried out clinical examinations. On the day of screening, children were made to sit on a wooden chair and intraoral examination was performed under natural daylight. Children identified with clinically missing permanent teeth or over-retained primary teeth were advised for radiographic examination to confirm the diagnosis of hypodontia. Information sheets, explaining the congenitally missing permanent teeth, duly signed by the class teacher along with informed consent forms for taking intraoral radiographs were sent to the respective parents.
| District name | No. of schools (govt. + private) | Children in govt. schools (girls + boys) | Children in private schools (girls + boys) | Total |
|---|---|---|---|---|
| Visakhapatnam | 4 (2 + 2) | 545 (213 + 332) | 561 (222 + 339) | 1,106 |
| Krishna | 4 (2 + 2) | 535 (208 + 327) | 551 (215 + 336) | 1,086 |
| Medak | 4 (2 + 2) | 538 (201 + 337) | 554 (210 + 344) | 1,092 |
| Mehboobnagar | 4 (2 + 2) | 534 (220 + 314) | 550 (227 + 323) | 1,084 |
| Rangareddy | 4 (2 + 2) | 533 (224 + 309) | 557 (233 + 324) | 1,090 |
| Total | 20 | 2,685 | 2,773 | 5,458 |
| Population type | Hypodontia cases (n) | Total population | % prevalence | p value |
|---|---|---|---|---|
| Girls | 42 | 2,173 | 1.9 | 0.497 |
| Boys | 36 | 3,285 | 1.1 | |
| Total | 78 | 5,458 | 1.4 |
An intraoral digital radiograph was taken using a portable X-ray unit (DX3000, Dexcowin, Korea) and a Kodak RVG system (5100, Carestream, France). All the students diagnosed with hypodontia were informed about their conditions and advised to seek dental treatment.
Statistical Analysis
Data obtained were tabulated and statistical analysis was performed using software “SPSS 21.0 and R environment ver.3.2.2”. A Chi-square test was applied to obtain the significance.
RESULTS
District-wise distribution of the study sample is displayed in Table 1. The total number of hypodontia cases reported in the estimated sample was 78 with an overall prevalence of 1.4% for both sexes combined (Table 2). Girls had a higher prevalence (1.9%) rate than boys (1.1%), this difference however was not statistically significant (p = 0.497).
Table 3 presents the frequency of hypodontia with respect to the individual tooth. The most frequently missing tooth was maxillary lateral incisor (44.54%), followed by mandibular incisors (26.30%) (central and lateral combined) and mandibular second premolar (19.0%). Cases with other missing teeth, except mentioned above, reported a smaller percentage. Maxilla was more frequently affected (52.5%) than the mandible (44.9%), but the difference was not significant (p = 0.45). Only 2.6% of hypodontia cases had both the jaws affected (Fig. 1). A non-significant, yet high prevalence of unilateral pattern (69.2%) of missing teeth (p = 0.10) and a predilection for the left side was observed (Figs 2 and 3).
A few salient findings of the present study were cases of missing mandibular incisors, maxillary premolars, and maxillary second molars. These teeth groups are otherwise not commonly reported to be missing in hypodontic patients, as per the global data. There were two cases with more than six teeth missing hence, they may be termed as “oligodontia”. The oligodontia cases in the present study were peculiar in that the maxillary lateral incisors and mandibular second premolars were found missing together. One case of a missing maxillary canine in a female subject was recorded.
DISCUSSION
Identification of hypodontia cases in a population with different ethnic/cultural backgrounds is not only important for national data but also for research purposes in the field of public health, anthropology, and the formulation of necessary treatment protocols. The etiology of hypodontia although is still not clear, has a multifactorial nature has been postulated. Besides genetics, environmental factors like endocrine disturbances, medical treatment, local pathology, and facial trauma have been implicated.11,18,19
In the present study, a genuine representation of the general population was considered. Institutional-based prospective studies20–23 or record-based retrospective studies on orthodontic patients4,24,25 have shown 1–2% overestimation in the prevalence of hypodontia when compared with cross-sectional studies conducted on the general population.18,26 Adolescents from five heavily populated districts in the states of Andhra Pradesh and Telangana were screened from both government and private schools to make the study sample inclusive of both low and high socioeconomic strata of the society. The age-group of 13 to 15 years was chosen, as the younger group would likely have more number of false-negative cases (late mineralization)18,26,27 or mixed dentition stage individual (exclusion criteria) and elder group might present with more number of false-positive cases due to addition of teeth lost for reasons other than agenesis. It has been reported in previous studies that clinical examination covers merely 58% of the actual number of cases of hypodontia.16,18,26,28 Hence, a dental radiograph was taken to confirm agenesis of the clinically missing tooth.
| Tooth number (FDI notation)* | n (%) | p value | ||
|---|---|---|---|---|
| Girls | Boys | Total | ||
| 12 | 17 (30.9) | 9 (16.4) | 26 (23.6) | 0.262 |
| 14 | 0 (0) | 1 (1.8) | 1 (0.9) | 0.5 |
| 15 | 1 (1.8) | 0 (0) | 1 (0.9) | 0.5 |
| 17 | 0 (0) | 1 (1.8) | 1 (0.9) | 0.5 |
| 22 | 11 (20.0) | 12 (21.8) | 23 (20.9) | 0.768 |
| 23 | 1 (1.8) | 0 (0) | 1 (0.9) | 0.5 |
| 24 | 1 (1.8) | 1 (1.8) | 2 (1.8) | 1 |
| 25 | 1 (1.8) | 2 (3.6) | 3 (2.7) | 0.414 |
| 27 | 0 (0) | 1 (1.8) | 1 (0.9) | 0.5 |
| 31 | 8 (14.5) | 5 (9.1) | 13 (11.8) | 0.431 |
| 32 | 1 (1.8) | 1 (1.8) | 2 (1.8) | 1 |
| 34 | 0 (0) | 1 (1.8) | 1 (0.9) | 0.5 |
| 35 | 7 (12.7) | 7 (12.7) | 14 (12.7) | 1 |
| 41 | 2 (3.6) | 8 (14.5) | 10 (9.1) | 0.16 |
| 42 | 3 (5.5) | 1 (1.8) | 4 (3.6) | 0.465 |
| 45 | 2 (3.6) | 5 (9.1) | 7 (6.4) | 0.577 |
* Federation Dentaire Internationale notation p value < 0.05 was considered statistically significant
The overall prevalence of hypodontia in our study was observed to be 1.4% as opposed to other Indian studies (4–16%).22,24,29–33 Global data also report a heterogeneity in the prevalence of hypodontia ranging from 0.3% in native Africans and Australian Aborigines to 36.5% in the Japanese population.18,26,28,34 This disparity may be attributed to variations in ethnic background, age-group of the samples, method of diagnosis, sample size, and sample type. Gender dimorphism was also revealed with a non-significant higher prevalence of hypodontia in girls (1.9%) than boys (1.1%) which may be attributed to sex hormones.2 Our finding is in accordance with other studies,5,8,18,20,25,35 although few have reported a higher prevalence in males.23,27,36

Fig. 1: Distribution of hypodontia according to jaw [p = 0.45 (NS)]

Fig. 2: Distribution of hypodontia according to pattern [p = 0.10 (NS)]
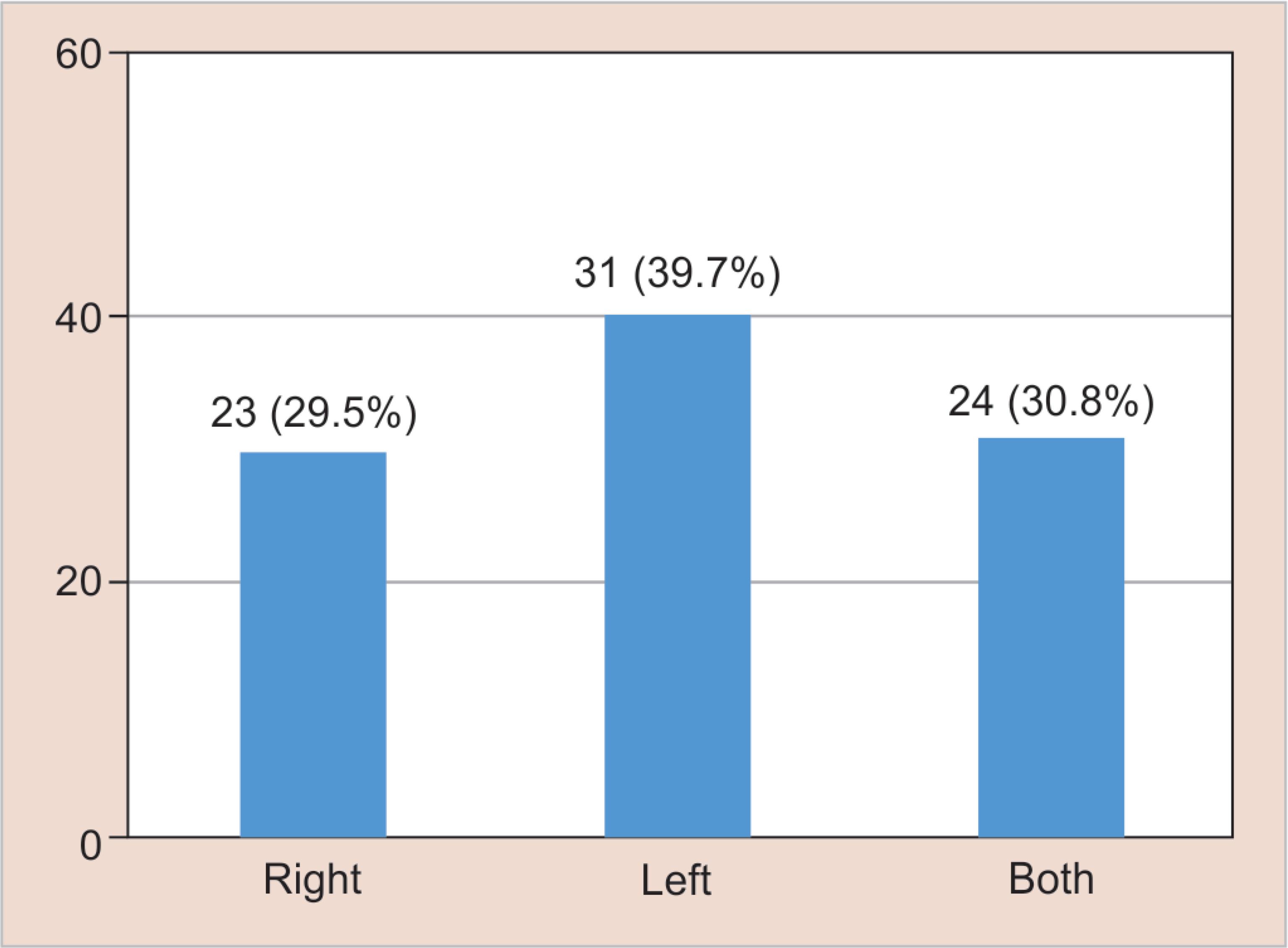
Fig. 3: Distribution of hypodontia according to side [p = 0.058 (NS)]
Various theories have been postulated to explain the etiology of the site-specific predilection of tooth agenesis. Butler’s field theory suggests four morphological fields (incisors, canines, premolars, and molars) in each jaw. The most mesial tooth in each field was proposed to be more genetically stable and therefore rarely missing while the teeth at end of each field are less genetically stable. Thus, the lateral incisors, second premolars, and third molars are the frequently missing teeth.3,37 A recent theory by Vastardis6 states that an evolutionary change is causing a gradual reduction in human dentition by the loss of an incisor, premolar, and molar in each quadrant. In the present study, the most frequently congenitally missing tooth was the maxillary lateral incisor which is in accordance with most of the Indian studies22,24,29–32 and few foreign studies,3,4,21,25,27,38 even though the majority of the studies have reported the mandibular second premolar to be the most commonly missing tooth.5,18,20,28,34–36,39,40 Often the maxillary lateral incisors and the mandibular second premolars are found missing together and this trait has been called “incisor premolar hypodontia” (IPH).1 Two cases of IPH were recorded in our study. Mandibular incisors and mandibular second premolars are also estimated to be frequently missing in our study. A non-significant higher prevalence (69.2%) of a unilateral pattern of a missing tooth was recorded which is in accordance with the observation of a meta-analysis study,18 however, few authors20,21,27,28 have reported the contrary. Among the unilateral cases, a predilection toward the left side and in the maxilla was noted. A similar observation has been reported by several authors25,27,38–40 though hypodontia with a predilection toward the right side3,20 and in mandible28,29 has also been reported.
A unique finding in the present study was a high percentage (26.3%) of cases with missing mandibular incisors, which is a characteristic of the Asian population.28,41 Pirinen et al.11 have introduced the term “recessively inherited incisor hypodontia” (RIH) and the trait is characterized by missing deciduous and permanent mandibular central and/or lateral incisors. The other uncommon findings of our study were cases with missing maxillary and mandibular second molars and maxillary canine.
An increase in the prevalence of hypodontia in recent times has been reported.37,42 However, there are no empirical data to support whether this finding is a consequence of the use of modern diagnostic tools with higher sensitivity and specificity or is there an actual increase in the frequency of gene mutation under the influence of the environment. To validate this finding, a periodic epidemiological survey should be conducted and probable cause is investigated.
LIMITATIONS OF THE STUDY
The present study did have a few limitations. First, it was difficult to precisely distinguish between the mandibular central and lateral incisor, especially when there were three incisors present and either well aligned or drifted. Second, the dental history recorded from children to rule out an incidence of dental extraction/avulsion might have been confounded by memory recall bias.
CONCLUSION
The present study reported an overall prevalence of 1.4% for non-syndromic hypodontia in the Indian population, with maxillary lateral incisor as the most frequently congenitally missing tooth. A higher prevalence rate was recorded in females and the most common pattern identified was unilateral, in the maxilla with a predilection for the left side. A considerably high percentage of congenitally missing mandibular incisors was recorded in the present study which could be an indigenous trait of the Indian population, thus necessitating further research.
REFERENCES
1. Arte S, Pirinen S. Hypodontia. Orphanet Encyclopedia 2004. 1–7.
2. Nunn JH, Carter NE, Gillgrass TJ, et al. The interdisciplinary management of hypodontia: background and role of paediatric dentistry. Br Dent J 2003;8(194 Suppl 5):245–251. DOI: 10.1038/sj.bdj.4809925.
3. Fekonja A. Hypodontia in orthodontically treated children. Eur J Orthod 2005;27(5):457–460. DOI: 10.1093/ejo/cji027.
4. Gomes RR, Calaca da Fonseca JA, Paula LM, et al. Prevalence of hypodontia in orthodontic patients in Brasilia, Brazil. Eur J Orthod 2010;32(3):302–306. DOI: 10.1093/ejo/cjp107.
5. Ajami B, Shabzendedar M, Mehrjerdian M. Prevalence of hypodontia in nine- to fourteen-year-old children who attended the Mashhad School of Dentistry. Indian J Dent Res 2010;21(4):549–551. DOI: 10.4103/0970-9290.74215.
6. Vastardis H. The genetics of human tooth agenesis: New discoveries for understanding dental anomalies. Am J Orthod Dentofacial Orthop 2000;117 (Suppl 6):650–656. DOI: 10.1016/S0889-5406(00)70173-9.
7. Parkin N, Elcock C, Smith RN, et al. The aetiology of hypodontia: The prevalence, severity and location of hypodontia within families. Arch Oral Biol 2009;54 (Suppl 1):52–56. DOI: 10.1016/j.archoralbio.2008.11.002.
8. Al-Ani AH, Antoun JS, Thomson WM, et al. Hypodontia: an update on its etiology, classification, and clinical management. Biomed Res Int 2017;2017:9378325. DOI: 10.1155/2017/9378325.
9. Dhanrajani PJ. Hypodontia: Etiology, clinical features, and management. Quintessence Int 2002;33(4):294–302.
10. Hobkirk JA, Gill DS, Jones SP, et al. Hypodontia: a team approach to management. Blackwell Publishing Ltd; 2011.
11. Pirinen S, Kentala A, Nieminen P, et al. Recessively inherited lower incisor hypodontia. J Med Genet 2001;38(8):551–556. DOI: 10.1136/jmg.38.8.551.
12. Tan PKS, Van Wijk AJ, Prahl-Andersen B. Severe hypodontia: identifying patterns of human tooth agenesis. Eur J Orthod 2011;33(2):150–154. DOI: 10.1093/ejo/cjq046.
13. Granhen H. Hypodontia in the permanent dentition: a clinical and genetical investigation. Odontol Rev 1956;7 (Suppl 3):77–78.
14. Pani SC. The genetic basis of tooth agenesis: Basic concepts and genes involved. J Indian Soc Pedod Prev Dent 2011;29(2):84–89. DOI: 10.4103/0970-4388.84677.
15. Townsend GC, Richards L, Hughes T, et al. Epigenetic influences may explain dental differences in monozygotic twin pairs. Aust Dent J 2005;50 (Suppl 2):95–100. DOI: 10.1111/j.1834-7819.2005.tb00347.x.
16. Larmour CJ, Mossey PA, Thind BS, et al. Hypodontia – A retrospective review of prevalence and etiology. Part I Quintessence Int 2005;36 (Suppl 4):263–270.
17. De Coster PJ, Marks LA, Martens LC, et al. Dental agenesis: genetic and clinical perspectives. J Oral Pathol Med 2009;38 (Suppl 1):1–17. DOI: 10.1111/j.1600-0714.2008.00699.x.
18. Polder BJ, Van’t Hof MA, Van der Linden FP, et al. A meta-analysis of the prevalence of dental agenesis of permanent teeth. Community Dent Oral Epidemiol 2004;32 (Suppl 3):217–226. DOI: 10.1111/j.1600-0528.2004.00158.x.
19. Brook AH. A unifying aetiological explanation for anomalies of human tooth number and size. Arch Oral Biol 1984;29(5):373–378. DOI: 10.1016/0003-9969(84)90163-8.
20. Kirzioğlu Z, Köseler Sentut T, Ozay Ertürk MS, et al. Clinical features of hypodontia and associated dental anomalies: a retrospective study. Oral Dis 2005;11 (Suppl 6):399–404. DOI: 10.1111/j.1601-0825.2005.01138.x.
21. Amini F, Rakhshan V, Babaei P. Prevalence and pattern of hypodontia in the permanent dentition of 3374 Iranian orthodontic patients. Dent Res J 2012;9(suppl 3):245–250.
22. Gupta SK, Saxena P, Jain S. Prevalence and distribution of selected developmental dental anomalies in an Indian population. J Oral Sci 2011;53 (Suppl 2):231–238. DOI: 10.2334/josnusd.53.231.
23. Guttal KS, Naikmasur VG, Bhargava P. Frequency of developmental dental anomalies in the Indian population. Eur J Orthod 2010;4(3):263–269.
24. Raju PS, Bhattacharya P. An epidemiological study of missing teeth among the North Indian population. Ann Essen Dentis 2011;3 (Suppl 2):11–14. DOI: 10.5368/aedj.2011.3.2.1.2.
25. Celikoglu M, Kazanei F, Miloglu O. Frequency and characteristics of tooth agenesis among an orthodontic patient population. Med Oral Patol Oral Cir Bucal 2010;15 (Suppl 5):e797–e801. DOI: 10.4317/medoral.15.e797.
26. Rakshan V. Meta-analysis and systematic review of factors biasing the observed prevalence of congenitally missing teeth in permanent dentition excluding third molars. Prog Orthod 2013;14(1):33–44. DOI: 10.1186/2196-1042-14-33.
27. Hedayati Z, Dashlibrun YN. The prevalence and distribution pattern of hypodontia among orthodontic patients in Southern Iran. Eur J Orthod 2013;7 (Suppl 1):78–82. DOI: 10.4103/1305-7456.119080.
28. Goya HA, Tanaka S, Maeda T, et al. An orthopantomographic study of hypodontia in permanent teeth of Japanese pediatric patients. J Oral Sci 2008;50 (Suppl 2):143–150. DOI: 10.2334/josnusd.50.143.
29. Soni HK, Joshi M, Desai H, et al. An orthopantomographic study of prevalence of hypodontia and hyperdontia in permanent dentition in Vadodara, Gujarat. Indian J Dent Res 2018;29 (Suppl 4):529–533. DOI: 10.4103/ijdr.IJDR_215_16.
30. Shetty P, Adyanthaya A, Adyanthaya S, et al. The prevalence of hypodontia and supernumerary teeth in 2469 school children of the Indian population: an epidemiological study. Indian J Stomat 2012;3 (Suppl 3):150–152.
31. Kathariya MD, Nikam AP, Chopra K, et al. Prevalence of dental anomalies among school going children in India. J Int Oral Health 2013;5 (Suppl 5):10–14.
32. Shankar D, Keshwar S, Verma N, et al. Prevalence of hypodontia in children of North Bihar: an orthopantomographic study. J Adv Med Dent Sci Res 2019;7 (Suppl 9):196–198.
33. Mukhopadhyay S, Mukhopadhyay P, Sarkar S, et al. Prevalence and distribution of hypodontia in a group of Bengali pediatric population. J Craniofac Max Dis 2015;4(1):28–32. DOI: 10.4103/2278-9588.151899.
34. Khalaf K, Miskelly J, Voge E, et al. Prevalence of hypodontia and associated factors: a systematic review and meta-analysis. J Orthod 2014;41 (Suppl 4):299–316. DOI: 10.1179/1465313314Y.0000000116.
35. Backman B, Wahlin YB. Variations in number and morphology of permanent teeth in 7-year-old Swedish children. Int J Paediatr Dent 2001;11(1):11–17. DOI: 10.1046/j.1365-263x.2001.00205.x.
36. Ng’ang’a RN, Ng’ang’a PM. Hypodontia of permanent teeth in a Kenyan population. East Afr Med J 2001;78 (Suppl 4):200–203. DOI: 10.4314/eamj.v78i4.9063.
37. Jorgenson RJ. Clinician’s view of hypodontia. J Am Dent Assoc 1980;101(2):283–286. DOI: 10.14219/jada.archive.1980.0186.
38. Sisman Y, Uysal T, Gelgor IE. Hypodontia. Does the prevalence and distribution pattern differ in orthodontic patients? Eur J Dent 2007;1(3):167–173. DOI: 10.1055/s-0039-1698333.
39. Hashem AA, O’ Connell B, Garvey T. Tooth agenesis in patients referred to an Irish tertiary care clinic for the developmental dental disorders. J Ir Dent Assoc 2010;56 (Suppl 2):23–27.
40. Rolling S. Hypodontia of permanent teeth in Danish school children. Scand J Dent Res 1980;88(5):365–369. DOI: 10.1111/j.1600-0722.1980.tb01240.x.
41. Davis PJ. Hypodontia and hyperdontia of permanent teeth in Hong Kong school children. Community Dent Oral Epidemiol 1978;15(4):218–220. DOI: 10.1111/j.1600-0528.1987.tb00524.x.
42. Mattheeuws N, Dermaut L, Martens G. Has hypodontia increased in caucasians during the 20th century? A meta-analysis. Eur J Orthod 2004;26(1):99–103. DOI: 10.1093/ejo/26.1.99.
________________________
© The Author(s). 2021 Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), which permits unrestricted use, distribution, and non-commercial reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.